Clinical Trial
Ethical approval for this study has been granted by South East Scotland REC.
Approval date: 02. 17-Jun-2021 / IRAS project ID: 291727 / REC reference: 21/SS/0028
Imaging is a key diagnostic procedure underpinning medical decisions in many clinical pathways. As a result, the number of imaging tests requested and performed in the National Health Service (NHS) has been rising year on year. Demand has outstripped resourcing in the NHS and there is currently a shortfall of over 1000 radiologists in the UK which will increase further by 2025. 98% of NHS Trusts are now unable to meet reporting within radiologists contracted hours (2018 Royal College of Radiologists workforce census) As a consequence, there is a rising backlog for reporting leading to delays in diagnosis and missed cancers as highlighted by the Care Quality Commission.
A better method of prioritisation for reporting of imaging tests is required to make better utilisation of expert radiologists and to minimise the impact of diagnostic delays in patient experience, management and outcome.
We think a computer-based ‘artificial intelligence’ (AI) system could be used to better triage chest radiographs than current methods in real-time so that the time to reporting for critical and urgent findings (irrespective of clinical history or referrer) can be reduced.
Our team have developed an AI system to detect a comprehensive set of 37 abnormalities in chest X-rays and have shown in a simulation its potential to reduce delays to reporting critical findings. Our initial work has found that the system greatly reduced the average “time to report” for critical examinations: 85% of the examinations labelled as critical would have been reported within the first day with the AI system, compared with 60% of the critical examinations reported from the historical data.
With improvements in system performance, AI may be a viable tool in improving how radiographs with important findings can be identified quickly, highlighted to an expert radiologist for confirmation of diagnosis, for a report to be issued to the clinician for actioning.
What is the purpose of this study?
We wish to test if AI triaging of chest X-rays in real time could potentially reduce the reporting time for radiographs with critical and urgent findings.
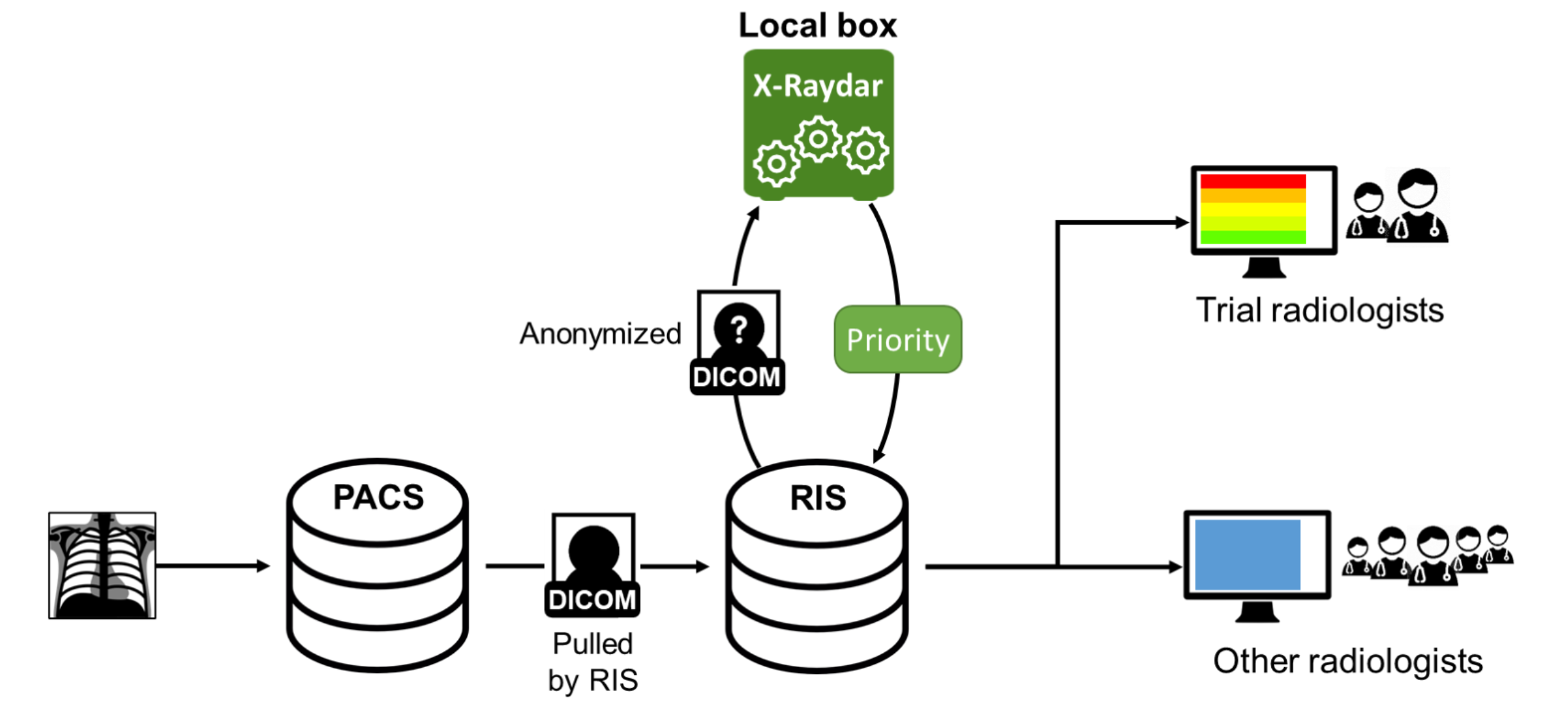
To do so, we integrated the prototype AI system on an existing PACS (Picture Archiving and Communication system) system of two major hospitals. Our AI system will process every chest X-ray acquired in these hospitals and will be integrated with the current reporting software used by radiologists. For each chest X-ray analysed by our system, the reporting software will receive an associated priority label in the ordered set {normal, non-urgent, urgent, critical}. This priority label will define the order in which the images should be reported, i.e. will provide a prioritization list.
In order assess the impact in the reporting time of our AI algorithm, the reporting time using the prioritisation list generated by the AI system for each category of radiograph (critical, urgent, non-urgent, normal) will be compared with the reporting time for the same category and the same radiologist before the implementation of the AI system on the PACS.
In order for the performance of the system in detecting critical and urgent findings to be checked, we will compare the priority label given by the AI system with the radiologists’ reports.
Trial Overview
Within each hospital there will be a set of radiologists using a modified working list of images to report. This working list will be sorted by our AI-based prioritization level.
To minimize the impact of this trial in the radiologists’ workflow, our system will be integrated with the current RIS software of each hospital, guaranteeing that any difference in the reporting time will be due to the AI-based prioritization.
Communication Overview
The chest X-rays of every participating hospital should be analysed by our AI algorithm. The algorithm will be the same for all the hospitals and will be hosted in an isolated server within each hospital.
Once the image is acquired in the hospital, the RIS provider will anonymize the DICOM file and send it to our AI server. Our server will reply with the AI-computed priority level. This priority level will then be added to the RIS software that will generate the priority-based sorted list for the radiologists participating in the trial.
The following figure summarizes the information shared between the different components involved in this study: